Related terms: CAD, coronary arteriosclerosis, coronary atherosclerosis, coronary heart disease, CHD, hardening of the arteries
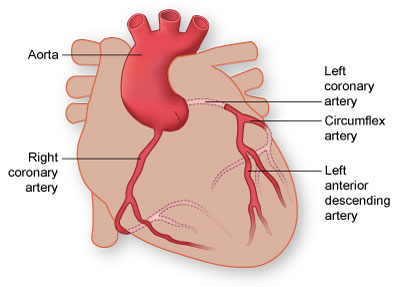 Coronary artery disease (CAD) affects more than 15 million Americans, making it the most common form of heart disease. CAD and its complications, like arrhythmia, angina pectoris, and heart attack (also called myocardial infarction), are the leading causes of death in the United States. CAD most often results from a condition known as atherosclerosis, which happens when a waxy substance forms inside the arteries that supply blood to your heart. This substance, called plaque, is made of cholesterol, fatty compounds, calcium, and a blood-clotting material called fibrin. Doctors have found that there are 2 kinds of plaque: hard and soft.
Coronary artery disease (CAD) affects more than 15 million Americans, making it the most common form of heart disease. CAD and its complications, like arrhythmia, angina pectoris, and heart attack (also called myocardial infarction), are the leading causes of death in the United States. CAD most often results from a condition known as atherosclerosis, which happens when a waxy substance forms inside the arteries that supply blood to your heart. This substance, called plaque, is made of cholesterol, fatty compounds, calcium, and a blood-clotting material called fibrin. Doctors have found that there are 2 kinds of plaque: hard and soft.
If hard plaque builds up in the arteries that supply blood to your heart, the blood flow slows or stops, preventing enough oxygen from getting to the heart, leading to a heart attack.
But doctors have now found that most heart attacks are caused by soft or vulnerable plaque. A vulnerable plaque is an inflamed part of an artery that can burst. This can lead to the formation of a blood clot, which can lead to heart attack.
See also on this site: Vulnerable Plaque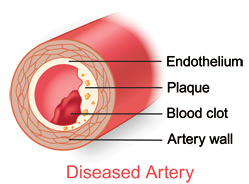
What causes atherosclerosis?
Scientists think the disease starts when the very inner lining of the artery (the endothelium) is damaged. High blood pressure, high levels of cholesterol and triglycerides in the blood, and smoking are believed to lead to the development of plaque.
What are the symptoms?
Atherosclerosis may be present for years without causing symptoms. This slow disease process can begin in childhood. In some people, the condition can cause symptoms by the time they reach their 30s. In others, they do not have symptoms until they reach their 50s or 60s. But, as the blockage gets worse, the slowed blood supply to the heart may begin to cause something called angina pectoris, chest pain.
For certain patients with CAD, angina may not be present. Sometimes the lack of oxygen to the heart (called ischemia) does not cause any pain, a condition known as silent ischemia.
How is CAD diagnosed?
Your doctor will take a medical history, ask about your symptoms, listen to your heart with a stethoscope, and perform certain tests, often including a chest x-ray. Here is a list of other tests that your doctor may order.
- An electrocardiogram (ECG or EKG) records your heart's electrical activity.
- A nuclear stress test uses a radioactive substance that is injected into your bloodstream to show how blood flows through your arteries.
- Echocardiography uses sound waves to produce an image of the heart to see how it is working.
- Coronary angiography is performed in the cardiac catheterization laboratory and gives doctors an x-ray "movie" of heart action and blood flow through your valves and arteries showing any blockages you may have.
- Positron emission tomography (PET) scanning uses information about the energy of certain elements in your body to show the parts of the heart muscle that are healthy or damaged.
How is CAD treated?
Medicines
A number of medicines can help relieve the angina pain that comes with CAD. People who have severe angina are often given a number of different medicines. Antiplatelet therapy, including aspirin, may also be given to patients with angina, because it decreases the chances of blood clots forming at the sites of the blockages.
- A medicine called nitroglycerin (nitro) can widen or dilate the arteries and improve blood flow to your heart.
- Beta-blockers "block" the chemical or hormonal messages sent to your heart that may cause it to work harder than it has to.
- Calcium channel blockers can help to keep your arteries open and reduce your blood pressure by relaxing the smooth muscle that surrounds the arteries in your body.
Percutaneous Interventions and Surgery
Because medicines cannot clear blocked arteries, a severely narrowed coronary artery may need more treatment to reduce the risk of a heart attack. Two major options are available: percutaneous interventions (also called transcatheter interventions) or coronary artery bypass surgery.
Both therapies have good track records among carefully selected patients. The decision to go with either option depends on how much narrowing there is, how many arteries are affected, the location of the narrowing, how much heart muscle is at risk, and individual patient factors, such as age and overall health.
Percutaneous Coronary Interventions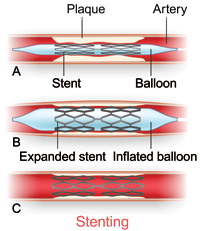
Angioplasty, which opens narrowed arteries, is performed by interventional cardiologists. They use a long, thin tube called a catheter that has a small balloon on its tip. They inflate the balloon at the blockage site in the artery to flatten the plaque against the artery wall. Angioplasty is also called percutaneous transluminal coronary angioplasty (PTCA).
A stent procedure is used along with balloon angioplasty. It involves placing a mesh-like metal device into an artery at a site narrowed by plaque. The opened stent keeps the vessel open and stops the artery from collapsing.
Some newer stents are covered with medicines that help keep the artery from closing up again. These are called coated stents or drug-eluting stents.
Atherectomy may be an option for certain patients who cannot have balloon angioplasty. A high-speed drill on the tip of a catheter is used to shave plaque from the artery walls.
Laser ablation uses a catheter that has a metal or fiberoptic probe on the tip. The laser uses light to "burn" away plaque and open the vessel enough so that a balloon can further widen the opening.
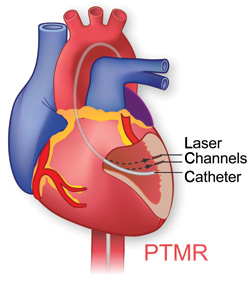 Percutaneous transmyocardial revascularization (PTMR) is performed by a cardiologist in the cardiac catheterization laboratory. After the area is numbed with anesthesia, the cardiologist inserts a catheter in an artery in the leg that leads to the heart. A laser is then fed through the catheter and used to create tiny holes in the heart muscle. These holes become channels for blood to flow to oxygen-starved areas of the heart. Researchers believe that the procedure may cause new vessels to form, reducing the pain of angina. PTMR is currently being used on patients who have not responded to other treatments such as medicines, angioplasty, or coronary artery bypass surgery.
Percutaneous transmyocardial revascularization (PTMR) is performed by a cardiologist in the cardiac catheterization laboratory. After the area is numbed with anesthesia, the cardiologist inserts a catheter in an artery in the leg that leads to the heart. A laser is then fed through the catheter and used to create tiny holes in the heart muscle. These holes become channels for blood to flow to oxygen-starved areas of the heart. Researchers believe that the procedure may cause new vessels to form, reducing the pain of angina. PTMR is currently being used on patients who have not responded to other treatments such as medicines, angioplasty, or coronary artery bypass surgery.
Surgery
Coronary artery bypass surgery involves "bypassing" blood flow around one or more narrowed vessels. To do this, the surgeon removes a vein or artery from another area of the body. This surgically removed vessel is called a graft. The graft may be cut into sections for use in routing blood flow around blocked coronary arteries. The surgeon connects a graft at points above and below the blockage to restore blood flow.
- Minimally invasive coronary artery bypass is a less invasive bypass surgery technique. The incision is smaller, and the procedure may be done while the heart is still beating. This reduces the risk of complications. The procedure may reduce patient recovery time, which decreases cost. This operation is only used for patients whose blockages can be bypassed through this smaller incision and whose risk of complications is low.
- Transmyocardial laser revascularization (TMLR) involves the use of a laser to create tiny channels in the lower left chamber of the heart (the left ventricle), which may increase blood flow within the heart. TMLR is only used on patients who have not responded to other treatments such as medicines, angioplasty, or coronary artery bypass surgery.
See also on this site:
See on other sites:
MedlinePlus
https://medlineplus.gov/coronaryarterydisease.html
Coronary Artery Disease
Updated August 2016